Treatments
Recurrent Candidiasis
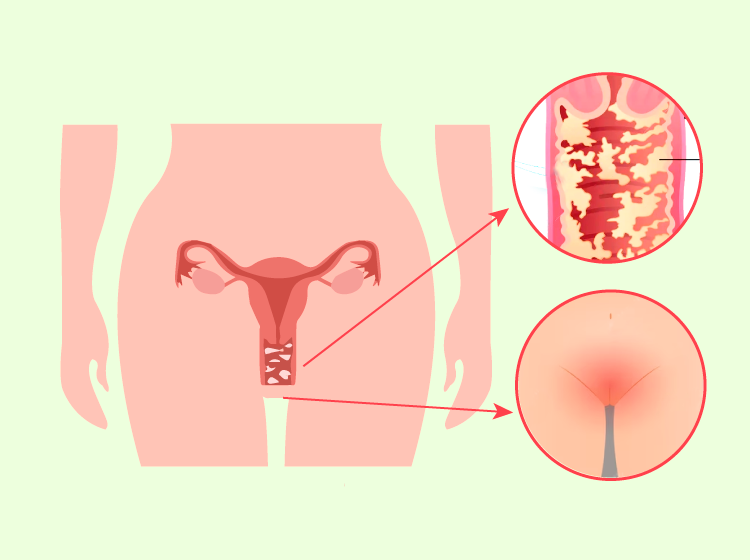
The fungus Candida albicans is responsible for the majority of vaginal yeast infections
The vagina naturally contains a balanced mixture of fungi, including Candida, and bacteria. Certain bacteria (Lactobacillus) act to prevent the overgrowth of fungi.
However, this balance can be disrupted, leading to an overgrowth of Candida or the penetration of the fungus into deeper cell layers, resulting in signs and symptoms of fungal vaginitis.
When is it considered recurrent candidiasis or chronic candidiasis?
We refer to recurrence in patients who experience four or more episodes of Candida vulvovaginitis per year.
These are patients who do not respond to medical treatment, have already corrected their hygiene habits, have been advised by their doctor to eliminate possible predisposing factors, have strengthened their microbiota, and have adopted healthy habits.
Despite all these measures, they continue to suffer from these bothersome episodes.
What symptoms and signs does candidiasis cause?
It is worth noting that vaginal yeast infections are not considered sexually transmitted diseases.
The symptoms can be mild and even go unnoticed by the patient or they can be very bothersome, affecting the quality of life of these women.
We may observe:
- Itching and irritation of the vulva and vagina
- Burning sensation, especially during sexual intercourse or urination
- Thick, white vaginal discharge that may have a clumpy appearance and no odor
- Redness and inflammation of the vulva and vagina
- Vaginal pain and discomfort
What situations can cause an overgrowth of vaginal yeast?
- The use of antibiotics, which disrupt the vaginal flora and promote the growth of Candida colonies.
- Pregnancy
- Diabetes
- A weakened immune system
- Stress
- Use of oral contraceptives or therapies with high estrogen levels
- Poor hygiene habits
- Use of daily panty liners
- Nylon underwear
What is the purpose of laser treatment?
Laser treatment is a very innovative, non-invasive, and painless option.
The laser has an immediate local fungicidal effect due to heat, and it also changes the environment, strengthening the flora.
It promotes neovascularization, which minimizes recurrence and improves the balance between fungi and normal bacteria.
The treatment is performed using the intravaginal device GYNA LUMIIA, which emits thermal energy. The patient may feel warmth, which is completely tolerable without the need for anesthesia.
The disappearance of vaginal infections has been observed as a beneficial side effect in patients who have undergone gynecological laser treatment for other symptoms such as vaginal dryness or urinary incontinence, among others.
When is vaginal laser indicated for the treatment of Candida?
When a vaginal infection is present, the first step is to perform a culture to identify the pathogenic agent and conduct an antibiotic susceptibility test to determine the most appropriate antibiotic at that time.
After receiving medication, oral probiotics should be added to repopulate the lost vaginal flora.
The patient should receive the necessary advice to correct any habits that may predispose her to these infections.
If the infection persists or recurs despite these measures, longer treatment periods can be considered.
If, after these measures, the tendency for infection persists or if the patient does not want or cannot be on medication for prolonged periods of time, then it is time to consider vaginal laser treatment.
Procedure
Laser sessions are performed at intervals according to the protocols. The number of sessions will depend on the individual patient's microbiota, age, previous treatments, and infection progression.
- No prior preparation is required.
- It is an outpatient procedure and painless.
- There are no post-procedure care instructions, except for abstaining from sexual activity for 72 hours.
- The patient can resume their usual activities on the same day.
We understand that this condition diminishes the quality of life, hinders the ability to have unrestricted sexual relations, and can distress the patient and sometimes their partners.
At Ginecolaser, we have the appropriate technology, extensive experience, and continuously improving results to help you solve the problem.
